Labour Induction – When, Why, and What to Expect
Introduction
Your due date has come and gone, and you’re eagerly awaiting the arrival of your little one. Or perhaps your healthcare provider has raised the possibility of bringing labor on sooner due to certain health concerns. In such situations, labour induction may be recommended.
But what exactly is labour induction?
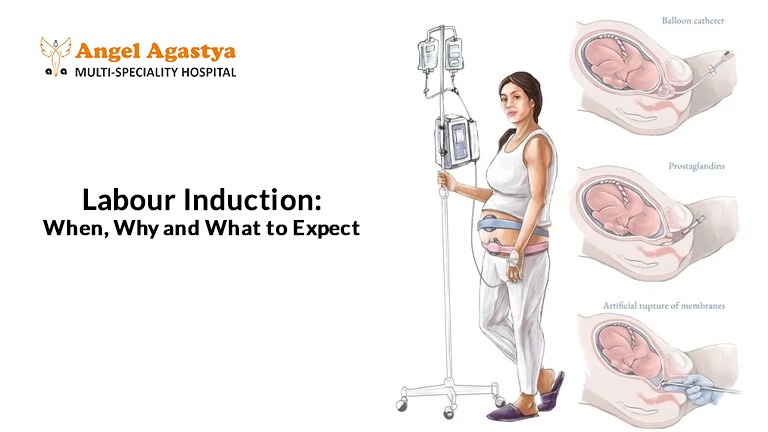
Labour induction is a medical procedure used to artificially stimulate uterine contractions to initiate childbirth. It’s a common, safe, and often necessary intervention when continuing the pregnancy poses a risk to the mother or baby. Knowing when labour induction is needed, the different methods involved, and what to expect can help ease anxiety and empower you to make informed decisions about your birth journey.
When is Labour Induction Necessary?
Labour induction is not done routinely. It is recommended only when delivering the baby is safer than continuing the pregnancy. Below are the common reasons when doctors may advise induction:

1. Post-Term Pregnancy
If your pregnancy crosses 41–42 weeks, it is considered overdue. After this point, the placenta may not function well, leading to reduced oxygen and nutrition to the baby.
Possible concerns include:
- Low amniotic fluid (less cushioning for the baby)
- Fetal distress (less oxygen supply)
- Macrosomia (very large baby, making normal delivery harder)
To avoid complications, doctors may suggest labour induction after 41 weeks. Regular check-ups and scans help decide the best time.
2. Health Conditions in the Mother
Some health issues can make early delivery a safer option:
- Pregnancy-Induced Hypertension (PIH) or Preeclampsia: High BP during pregnancy can cause seizures or affect blood flow to the baby.
- Gestational Diabetes: Uncontrolled sugar levels can lead to a big baby or rarely, stillbirth.
- Other medical conditions like liver problems (cholestasis), kidney issues, or long-standing illnesses may also require timely labour induction.
3. Baby’s Health Concerns
If your baby shows signs of distress or slow growth, labour induction may be needed:
- Fetal Growth Restriction (FGR): Baby is smaller than expected due to poor placenta function.
- Low amniotic fluid (Anhydramnios): Can affect the baby’s movements and cord safety.
- Abnormal heartbeat patterns seen during monitoring may mean the baby is under stress and needs to be delivered soon.
4. Premature Rupture of Membranes (PROM)
If your water breaks but labour doesn’t start within 24–48 hours, there’s a risk of infection. In such cases, doctors usually begin labour induction to keep both mother and baby safe.
5. Elective Induction (Planned for Convenience)
Some women ask for labour induction for personal reasons—like staying near the hospital or managing family support. This is only considered safe after 39 weeks and if the cervix is ready for labour.
How is Labour Induction Performed?
Labour induction is the process of stimulating contractions before natural labor begins, with the goal of delivering the baby safely. It’s recommended when continuing the pregnancy poses more risks than benefits to the mother or baby. Several methods are available for labour induction, and the choice depends on factors like cervical readiness, gestational age, overall health, and the medical reason for labour induction.
Cervical Readiness – The Bishop Score
Before selecting a labour induction method, your healthcare provider will assess your cervix using the Bishop Score, a scoring system that helps predict the success of labour induction. It evaluates five key factors:
- Dilation – how open the cervix is (measured in centimeters)
- Effacement – how thin or stretched the cervix has become
- Consistency – whether the cervix feels firm, medium, or soft
- Position – whether the cervix is positioned toward the back (posterior) or front (anterior)
- Fetal Station – how far the baby has moved down into the pelvis
Each factor is given a score, and the total helps determine whether the cervix is “favorable” for labour induction.
A higher Bishop Score (usually 8 or more) suggests the cervix is ready for labour induction and increases the chances of a smooth and successful outcome. If the score is low, your doctor might recommend methods to ripen the cervix first, such as medications or mechanical dilation, before starting induction.
Methods of Labour Induction
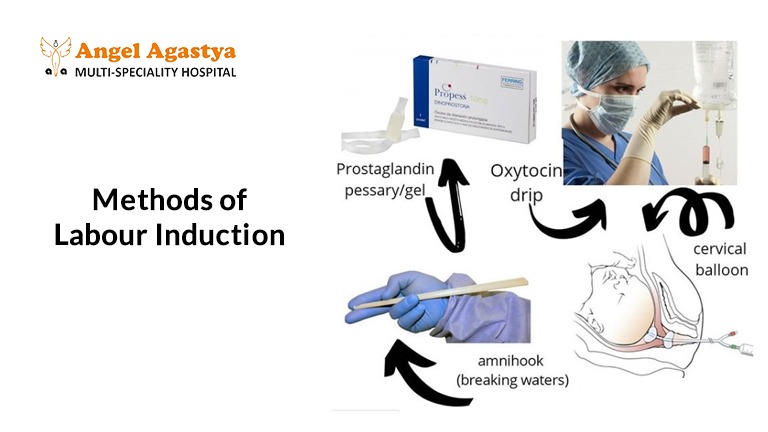
1. Non-Medical Methods
Used when a gentle start to labour induction is needed:
Membrane Sweeping: The doctor carefully separates the water bag from the uterus during an internal check-up to help start labour.
Nipple Stimulation: Rubbing or massaging the nipples helps release natural oxytocin, which can bring on contractions.
2. Medical Methods
These use medicines to soften the cervix or start contractions:
Cervidil: A vaginal tablet that slowly releases hormones.
Misoprostol (Cytotec): Given by mouth or vaginally to soften the cervix.
Oxytocin (Pitocin): Given through a drip in the hand.
The dose is slowly increased to bring regular contractions.
3. Mechanical Methods
These help open the cervix physically:
Foley Catheter: A balloon is placed in the cervix and gently inflated to help it open.
Laminaria: Sticks made from dried seaweed are placed in the cervix where they swell and help open it slowly.
4. Amniotomy (Water Breaking)
If the cervix is partly open, the doctor may break the water using a sterile tool to speed up labour induction.
5. Combination Methods
Often, more than one method is used—for example, medicines to soften the cervix first, followed by oxytocin to make labour induction.
What to Expect During Labour Induction
Every woman’s experience with labour induction is different, depending on her body and the methods used. Here’s what typically happens:
1. Monitoring
- You’ll be closely monitored to track fetal heart rate and contraction patterns.
- Your vital signs will be checked regularly to ensure everything is progressing safely.
2. Contractions
- Induced contractions may feel stronger and come on more suddenly than natural ones.
- You might feel more discomfort earlier in the process, especially if your cervix isn’t already dilated.
3. Pain Relief Options
You have access to all the usual pain relief options:
- Epidural anesthesia
- Nitrous oxide (laughing gas)
- IV pain medications
- Breathing techniques, massage, and labor support
Always discuss your preferences with your birth team.
4. Labour Duration
The time it takes varies:
- If your cervix is already soft and partly dilated, labor may progress quickly.
- If it’s not yet favorable, the process could take 12 to 48 hours or more.
5. Risk of Longer or Failed Induction
Sometimes, induction takes longer than expected. In certain cases, labor may not progress, and a cesarean birth may become necessary for the safety of the mother and baby.
6. Emotional Considerations
It’s normal to feel anxious, frustrated, or overwhelmed. Talk to your support team and stay informed. Having a birth plan can help manage expectations.
Risks and Considerations of Labour Induction
While generally safe, labour induction carries some potential risks:
1. Cesarean Delivery
There’s a slightly higher chance of needing a cesarean, especially for:
- First-time mothers
- Unfavorable cervix at the time of induction
2. Uterine Hyperstimulation
Induction drugs like oxytocin can sometimes cause overly frequent or strong contractions, which may reduce oxygen flow to the baby.
3. Fetal Distress
Close monitoring is essential. If the baby shows signs of distress, interventions like cesarean delivery may be necessary.
4. Infection
The longer the time between water breaking and delivery, the higher the risk of infection, especially with procedures like amniotomy.
5. Uterine Rupture (Rare)
A very rare but serious complication, especially in women with a prior cesarean section or uterine surgery.
6. The Importance of Informed Consent
Before starting the induction, ensure your healthcare provider discusses:
- Why it’s being recommended
- Methods being used
- Potential risks and alternatives
You have the right to ask questions, understand your options, and give informed consent.
Conclusion
Labour induction is a safe and commonly done medical step that doctors may recommend when it’s better for the baby or mother not to wait for natural labour. This might happen if your due date has passed, if there are any health concerns (like high blood pressure or diabetes), or if your doctor feels the baby isn’t growing well inside the womb. In such cases, inducing labour can help avoid risks and ensure a safe delivery.
It’s important for expecting mothers and families to understand why labour may need to be induced, what methods are used (like medicines, drips, or small procedures to help start contractions), and what possible side effects or challenges may come up. Some women may feel more pain during induced labour, or it may take longer—so being mentally and physically prepared makes a big difference.
Always have open conversations with your gynaecologist or delivery team. Ask questions, clarify doubts, and share your preferences. When you’re informed and involved in the process, you feel more confident, calm, and ready to welcome your little one in the best possible way.
Frequently Asked Questions (FAQs)
1. Does labour induction hurt more than natural labor?
Induced contractions can feel more intense for some women, but pain is subjective. Pain relief options like epidurals and breathing techniques can help manage discomfort.
2. Can I still have a vaginal birth after induction?
Yes. The goal of induction is a vaginal birth. However, if complications arise, a cesarean might be needed.
3. How can I prepare for a possible induction?
Learn about the process, discuss with your doctor, and prepare mentally and physically for labour induction.
4. How long does induction take?
It varies widely. It may take a few hours to over 24 hours depending on the cervix’s readiness and response to the induction methods.
5. Will I be able to move around during induction?
That depends on the type of monitoring used. Wireless or intermittent monitoring may allow more mobility—discuss this with your provider.
6. Are there natural ways to induce labor?
Some suggest walking, spicy food, or nipple stimulation. However, these aren’t guaranteed and should always be discussed with a healthcare provider first.
7. What if I don’t want to be induced?
You have the right to decline. Have an open conversation with your doctor about the risks and alternatives.
8. Is elective induction riskier?
Elective induction after 39 weeks is considered safe when done correctly, but it may carry a slightly higher cesarean risk, especially for first-time moms.
9. Will my baby be safe if I’m induced?
Yes, labour induction is recommended only when it’s considered the safest option for you and your baby. Monitoring ensures safety throughout.
10. What happens after a successful induction?
Postpartum recovery is similar to a spontaneous delivery. Focus on rest, bonding with your baby, and following up on postnatal care.

