Introduction:
The female reproductive system undergoes a complex series of changes throughout life, influenced by hormonal fluctuations. While experiencing irregular or abnormal vaginal bleeding is a common occurrence for many women, particularly during their reproductive years, it’s crucial to address any significant deviations from your typical menstrual pattern. In such situations, an endometrial biopsy emerges as a vital diagnostic tool, offering valuable insights into the health of the uterine lining and aiding in the timely diagnosis and management of various uterine abnormalities.
Common Reasons for Endometrial Biopsy:
Endometrial biopsy extends beyond simply investigating abnormal bleeding. It serves as a cornerstone for accurate assessment in various clinical scenarios:
- Abnormal Uterine Bleeding: This encompasses a spectrum of irregularities, including:
- Heavy menstrual bleeding (menorrhagia): Periods exceeding seven days or requiring frequent pad/tampon changes.
- Intermenstrual bleeding (metrorrhagia): Bleeding occurring between menstrual cycles.
- Prolonged bleeding (menometrorrhagia): Continuous or frequent bleeding exceeding eight days.
- Postmenopausal bleeding: Any bleeding after menopause requires investigation, regardless of amount or frequency.

- Unexplained Infertility: Endometrial biopsy can assist in identifying potential causes of infertility, such as endometrial polyps, which can impede implantation, or abnormal endometrial receptivity, affecting embryo attachment.
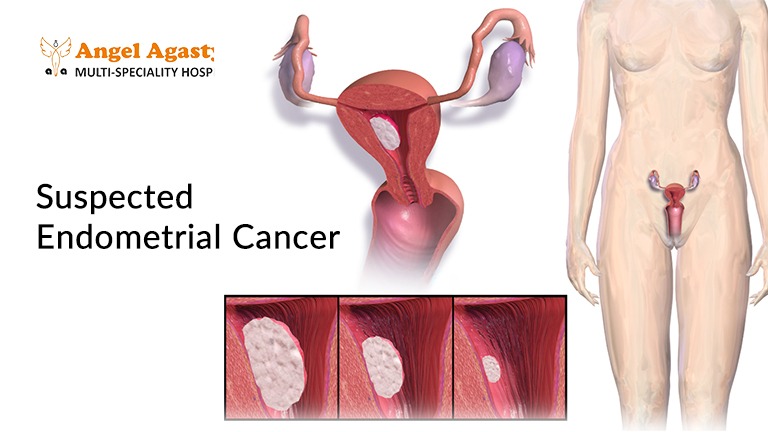
- Suspected Endometrial Cancer: In situations where endometrial cancer is suspected based on patient history, imaging findings (ultrasound, hysteroscopy), or other clinical features, biopsy becomes crucial for definitive diagnosis. Early detection is critical for achieving optimal treatment outcomes.
- Monitoring Hormonal Therapy Response: Endometrial biopsy can assess the impact of hormonal therapy, such as tamoxifen used for breast cancer treatment, on the endometrium, as it can potentially increase the risk of endometrial cancer.

- Evaluation of Abnormal Thickening on Imaging: Transvaginal ultrasound or hysterosalpingography may reveal thickened endometrium, which deviates from the expected normal range. Further investigation through biopsy helps rule out underlying pathologies, including polyps or hyperplasia.
Benefits of Endometrial Biopsy:
Endometrial biopsy offers a multitude of advantages over other diagnostic techniques:
- Early Diagnosis and Treatment: Early detection of potential issues like endometrial cancer or precancerous conditions allows for prompt intervention and improved disease management, significantly enhancing the chances of successful treatment.
- Minimally Invasive: Compared to traditional surgical techniques like dilation and curettage (D&C), biopsy offers a safer and more comfortable experience with minimal patient discomfort. It can be performed in an outpatient setting, allowing patients to return home after the procedure.
- Accurate Diagnosis: Biopsy provides definitive information about the underlying cause of symptoms, guiding appropriate treatment plans and avoiding unnecessary procedures or medications.
- Targeted Approach: In situations requiring further evaluation, biopsy can be coupled with hysteroscopy, allowing for visualization of the uterine cavity and targeted tissue collection from specific areas of concern.
When to Consider an Endometrial Biopsy:
While every woman’s body is unique, consulting a healthcare provider if you experience any of the following is crucial:
- Abnormal uterine bleeding: This includes any significant change in the frequency, duration, or amount of bleeding compared to your typical menstrual pattern.
- Postmenopausal bleeding: Any vaginal bleeding after menopause, regardless of the amount or frequency, requires investigation.
- Pelvic pain or discomfort: While not always associated with endometrial abnormalities, persistent pelvic pain can warrant further evaluation.
- Unexplained infertility: If you haven’t gotten pregnant after a year of trying consistently or after six months if you’re 35 years or older, discussing your fertility concerns with your healthcare provider is crucial.
Open communication and exploring your concerns during consultations with healthcare professionals can ensure timely diagnosis and appropriate management strategies.
Summary:
Endometrial biopsy emerges as a pivotal tool in the diagnostic armamentarium of healthcare professionals, offering valuable insights into the health of the uterine lining. Its ability to provide accurate and timely information regarding potential underlying conditions facilitates early diagnosis and effective treatment planning, empowering optimal women’s health and well-being.
Endometrial biopsy holds immense significance in safeguarding women’s health by enabling accurate and timely diagnosis of various uterine abnormalities. Its minimally invasive nature and capacity to provide definitive information empower healthcare professionals to develop appropriate treatment plans and optimize patient outcomes. By understanding the purpose, process, and potential benefits of this crucial diagnostic tool, women and their healthcare providers can work collaboratively to ensure their overall well-being.
FAQs:
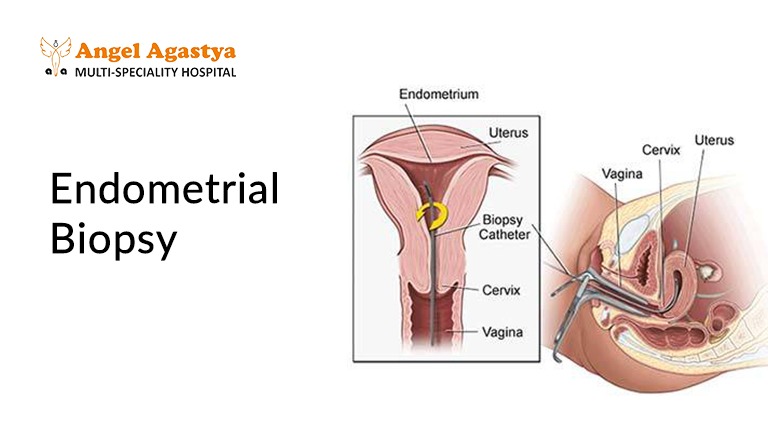
1. What happens during an endometrial biopsy?
Endometrial biopsy typically involves inserting a thin tube or instrument through the cervix and into the uterine cavity to collect a small tissue sample. Depending on the chosen technique, the sample might be aspirated, brushed, or directly grasped and removed. The procedure is usually performed in a clinic setting and is generally well-tolerated, although mild cramping or discomfort may be experienced.
2. What are the risks associated with endometrial biopsy?
While generally safe, potential complications can occur, including:
- Bleeding: Mild vaginal bleeding is expected after the procedure and typically resolves within a few days.
- Infection: The use of prophylactic antibiotics minimizes this risk, but infection remains a possibility.
- Uterine perforation: This is a rare but serious complication where the biopsy instrument accidentally punctures the uterine wall.
- Cramping: Mild cramping similar to menstrual cramps is common and can be managed with pain medication.
3. How long does it take to recover from an endometrial biopsy?
Most women can resume their usual activities within a day. Still, strenuous exercise or heavy lifting should be avoided for a short period (typically 24-48 hours) as advised by the healthcare provider.
4. What are the different types of endometrial biopsy?
Several types of endometrial biopsy exist, each with its advantages and limitations:
- Aspiration biopsy: Utilizes a suction device to collect a sample, minimally invasive but may not be ideal for obtaining large tissue samples.
- Pipelle biopsy: A disposable, flexible tube with a cutting port, offering easy use and effective tissue acquisition.
- Endometrial brush biopsy: Employs a soft brush to collect loose cells, primarily used for evaluating endometrial hyperplasia or monitoring hormonal therapy response.
- Hysteroscopic biopsy: Involves using a hysteroscope to visualize the uterine cavity and obtain targeted biopsies, requiring specialized equipment and expertise.
5. How do I prepare for an endometrial biopsy?
Preparation typically involves a detailed medical history review, physical examination, and discussion of the procedure with the healthcare provider. Depending on individual situations, taking medications like antibiotics or pain medication beforehand might be recommended.
6. What are the potential results of an endometrial biopsy?
The collected tissue sample undergoes microscopic examination by a pathologist to determine the presence and nature of any abnormalities. Possible findings include:
- Normal endometrium: The tissue exhibits the expected structural features for the patient’s age and menstrual cycle phase.
- Endometrial hyperplasia: An abnormal thickening of the lining, categorized based on severity (simple, complex, atypical), potentially requiring further evaluation or treatment.
- Endometrial cancer: Various types of endometrial cancer can be identified, each with specific treatment plans.
- Other benign conditions: Endometrial polyps, stromal endometriosis, or benign inflammatory processes may be detected.
- Inconclusive findings: In rare cases, the biopsy may not provide definitive results, necessitating repeat biopsy or other diagnostic modalities.
7. Who should not undergo an endometrial biopsy?
Endometrial biopsy is generally not recommended for women who are pregnant, have an active pelvic infection, or have an anatomically distorted uterus which makes safe insertion of the biopsy instrument challenging.
8. What are the alternatives to an endometrial biopsy?
Depending on the specific situation, alternative diagnostic options might exist. These could include:
- Ultrasound: Can assess the thickness of the endometrium and identify potential abnormalities, however, it cannot provide a definitive diagnosis.
- Hormonal testing: This may be used to investigate potential hormonal imbalances contributing to abnormal bleeding.
- Endometrial cytology: This involves analyzing cells shed from the endometrium, but it’s less accurate than biopsy and may miss certain abnormalities.
9. Will I need further treatment after an endometrial biopsy?
The need for further treatment depends entirely on the biopsy results.
Depending on the biopsy results, there are different paths we can take to address the situation. Some options may include:
- Hormonal therapy: Medications like birth control pills or progestin therapy can regulate menstrual cycles and manage abnormal bleeding.
- Surgery: Surgical removal of polyps or other benign growths may be necessary.
- Cancer treatment: If the biopsy confirms endometrial cancer, specific treatment plans are formulated based on the cancer type and stage.
10. What if I have more questions about an endometrial biopsy?
It’s always crucial to address any concerns you have with your healthcare provider. They can provide personalized information and guidance regarding the procedure, potential risks, and benefits, and answer any specific questions you may have based on your circumstances. Remember, open communication and shared decision-making are vital throughout the diagnosis and treatment process.


I am extremely impressed with your writing skills as well
as with the layout on your weblog. Is this a paid
theme or did you customize it yourself? Either way keep up the
excellent quality writing, it is rare to see a great blog
like this one nowadays.
Thanks for your kind words! Free theme + customizable. Soon we will come up with a more updated version.