PCOS and Long-Term Health Risks: Safeguarding Your Future Health
Hook:
For many women, Polycystic Ovary Syndrome (PCOS) is more than just a reproductive issue; it’s a lifelong health challenge that can increase the risk of numerous serious conditions. Addressing PCOS early is not just about managing its immediate symptoms—it’s about taking proactive steps to safeguard your long-term health.
Introduction
Polycystic Ovary Syndrome (PCOS) affects millions of women across the globe and is often recognized for its impact on fertility and reproductive health. However, the implications of PCOS go far beyond irregular periods or trouble conceiving. PCOS can have a cascading effect on long-term health, increasing the risk of chronic diseases such as cardiovascular issues, type 2 diabetes, and even certain types of cancer. As such, managing PCOS is not just about addressing immediate symptoms but also about preventing severe long-term health complications. This guide explores the various long-term health risks associated with PCOS and how women can take steps today to reduce their risk for tomorrow.
Section 1: PCOS and Metabolic Syndrome
Understanding Metabolic Syndrome
Metabolic syndrome is a group of conditions that collectively increase the risk of developing heart disease, stroke, and type 2 diabetes. These conditions include high blood pressure, high blood sugar levels, excess abdominal fat, and abnormal cholesterol or triglyceride levels. Women with PCOS are particularly vulnerable to metabolic syndrome due to hormonal imbalances and insulin resistance, both of which are hallmark features of PCOS.
The Link Between PCOS and Metabolic Syndrome
The hormonal disturbances associated with PCOS, particularly elevated androgens and insulin resistance, contribute to the development of metabolic syndrome. Insulin resistance can lead to hyperinsulinemia (excess insulin in the blood), which in turn increases fat storage, particularly around the abdomen. This visceral fat accumulation is a significant risk factor for metabolic syndrome. Moreover, the higher levels of androgens in women with PCOS can worsen insulin sensitivity, creating a vicious cycle of weight gain and metabolic disturbance.
Increased Risk of Health Complications
Women with both PCOS and metabolic syndrome are at a significantly higher risk of severe health conditions. The likelihood of developing type 2 diabetes is nearly quadrupled, while the risk of heart disease and stroke is also substantially increased. Addressing metabolic syndrome through lifestyle changes and medication is crucial for preventing long-term complications.
Section 2: PCOS and Cardiovascular Disease
Risk Factors for Cardiovascular Disease
Cardiovascular disease is a major health concern for women with PCOS. Several risk factors, including insulin resistance, high cholesterol, high blood pressure, and chronic inflammation, are prevalent in women with this condition. High levels of androgens further contribute to the development of atherosclerosis (the buildup of fatty deposits in the arteries), which can lead to heart attacks and strokes.
The Impact of Chronic Inflammation
Inflammation plays a central role in the progression of cardiovascular disease. Women with PCOS often have elevated markers of inflammation, such as C-reactive protein (CRP), which can exacerbate the risk of heart disease. Chronic inflammation can damage blood vessels and promote the development of plaques in the arteries, further increasing cardiovascular risk.
Preventive Measures for Heart Health
Preventing cardiovascular disease requires a multifaceted approach. First, it’s important to manage underlying conditions such as insulin resistance, high blood pressure, and cholesterol. Regular exercise and a diet rich in heart-healthy foods like vegetables, lean proteins, and whole grains can help mitigate these risks. Women with PCOS should also avoid smoking and manage stress levels, as both of these factors can significantly impact heart health.
Section 3: PCOS and Type 2 Diabetes
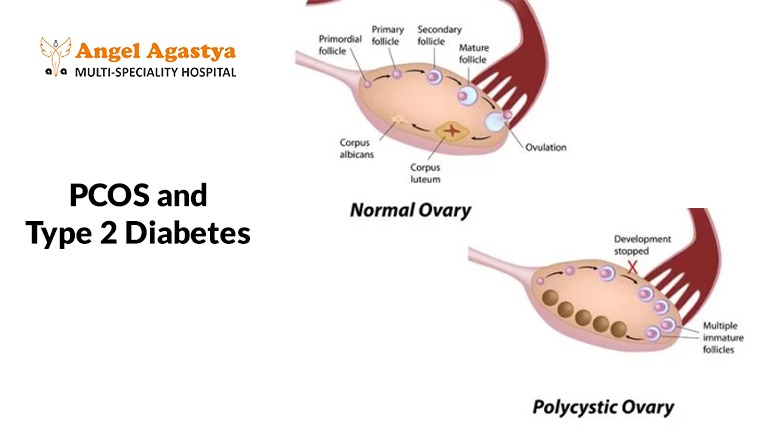
The Role of Insulin Resistance
Insulin resistance is a key feature of PCOS and is one of the leading causes of type 2 diabetes in women with the condition. Insulin is your body’s blood sugar regulator, helping cells absorb glucose. In women with PCOS, the cells become less responsive to insulin, leading to elevated blood sugar levels and eventually diabetes.
Monitoring and Managing Blood Sugar Levels
Regular monitoring of blood sugar levels is critical for women with PCOS, especially those with insulin resistance. Early detection of prediabetes or diabetes can help prevent long-term complications. Dietary changes, such as reducing sugar intake and consuming complex carbohydrates, are essential for maintaining stable blood sugar levels. In some cases, medications like metformin, which improves insulin sensitivity, may be prescribed to help manage glucose levels.
The Importance of Weight Management
A healthy weight is your best defense against type 2 diabetes. Even modest weight loss can significantly improve insulin sensitivity and blood sugar control. Regular physical activity, including aerobic exercises and strength training, can also enhance insulin sensitivity and support long-term metabolic health.
Section 4: Other Long-Term Health Risks
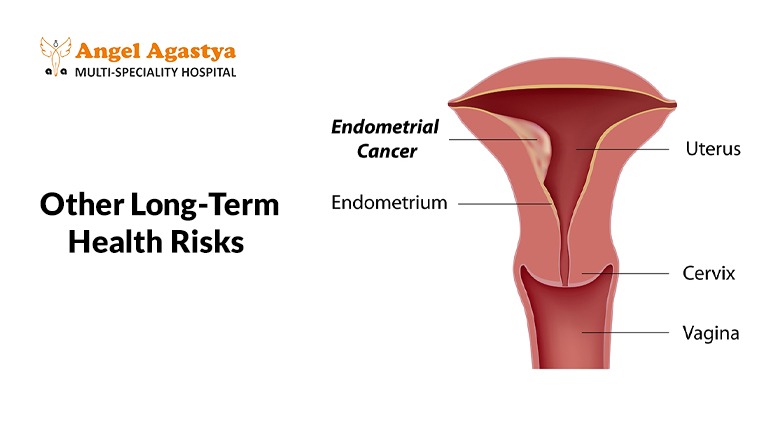
Endometrial Cancer
Women with PCOS are at an increased risk of developing endometrial cancer due to prolonged exposure to unopposed estrogen. Irregular or absent periods can lead to a buildup of the uterine lining, which can become cancerous over time. Regular monitoring and, in some cases, hormone therapy to regulate menstrual cycles can help reduce this risk.
Sleep Apnea
Sleep apnea is another health risk for women with PCOS, particularly those who are overweight or obese. This condition, characterized by pauses in breathing during sleep, can lead to poor-quality sleep, daytime fatigue, and an increased risk of cardiovascular disease. Sleep apnea is also associated with insulin resistance, further exacerbating the risk of type 2 diabetes.
Mental Health Concerns
PCOS can take a toll on mental health, contributing to anxiety, depression, and poor self-esteem. The physical symptoms of PCOS, such as weight gain, acne, and excess hair growth, can affect body image and lead to emotional distress. It’s important for women with PCOS to seek support for their mental health, whether through counseling, therapy, or support groups.
Section 5: Preventive Steps for Long-Term Health

Lifestyle Modifications
Adopting a healthy lifestyle is the cornerstone of managing PCOS and preventing long-term health complications. A balanced diet that includes plenty of fruits, vegetables, whole grains, and lean proteins can help manage insulin resistance and reduce the risk of cardiovascular disease. Regular physical activity, including both aerobic exercises and strength training, is essential for maintaining a healthy weight and improving insulin sensitivity.
Managing Stress and Sleep
Chronic stress can exacerbate PCOS symptoms and increase the risk of long-term health complications. Incorporating stress-reducing activities, such as yoga, meditation, or deep breathing exercises, can have a positive impact on both mental and physical health. Additionally, getting adequate sleep is crucial for overall well-being. Women with PCOS should aim for 7-9 hours of sleep per night and consider seeking treatment for sleep apnea if needed.
Medical Interventions
In some cases, medical interventions may be necessary to manage PCOS and reduce the risk of long-term complications. Hormonal birth control, for example, can help regulate menstrual cycles and reduce the risk of endometrial cancer. Medications like metformin can improve insulin sensitivity and lower the risk of type 2 diabetes. Regular check-ups with a healthcare provider are essential for monitoring health and addressing any emerging risks.
Conclusion
PCOS is more than a reproductive condition—it’s a complex health issue that can increase the risk of several long-term health problems, including cardiovascular disease, type 2 diabetes, and certain cancers. By understanding the connection between PCOS and these long-term risks, women can take proactive steps to manage their condition and reduce the likelihood of serious health complications. Lifestyle changes, regular medical monitoring, and appropriate treatments can make a significant difference in improving health outcomes for women with PCOS.
FAQs
- Can PCOS lead to heart disease?
Yes, PCOS can increase the risk of heart disease due to its association with insulin resistance, high cholesterol, and high blood pressure.
2. What are the early signs of type 2 diabetes?
Watch out for these early warning signs: increased thirst, frequent trips to the bathroom, feeling tired, and blurry vision.
3. How can I reduce my risk of endometrial cancer with PCOS?
Maintaining a healthy weight, regulating menstrual cycles with medication, and regular monitoring can reduce the risk.
4. What are the symptoms of sleep apnea?
If you snore loudly, stop breathing during sleep, or feel excessively sleepy during the day, you might have sleep apnea.
5. Can PCOS affect mental health?
Yes, PCOS can contribute to anxiety, depression, and low self-esteem.
6. What lifestyle changes can help prevent long-term health complications associated with PCOS?
Adopting a healthy diet, regular exercise, managing stress, and maintaining a healthy weight are key lifestyle changes.
7. Are there medications to manage PCOS and reduce the risk of health problems?
Yes, medications like metformin and hormonal birth control can help manage PCOS and reduce associated risks.
8. How often should I see a doctor for regular check-ups if I have PCOS?
It’s important to see a doctor at least once a year, or more frequently if you have additional health concerns.
9. Can PCOS be reversed?
PCOS cannot be reversed, but symptoms can be managed effectively with lifestyle changes and medication.
10. What are the long-term health implications of untreated PCOS?
Untreated PCOS can lead to serious conditions like heart disease, type 2 diabetes, endometrial cancer, and mental health issues.
