What is High-Risk Pregnancy?

This powerful guide reveals the critical signs that could indicate a high-risk pregnancy, alongside expert advice on how to navigate these challenges. Whether you’re planning for the future or currently expecting, learn the essential steps you can take to protect both you and your baby. Don’t miss out on crucial insights—empower yourself with knowledge today!
Introduction
Pregnancy is a joyous journey for most women, but for some, it can present unique challenges. A high-risk pregnancy refers to a pregnancy that carries an increased risk of complications for the mother, the fetus, or both. These complications can range from mild to severe and may require specialized medical care and monitoring throughout the pregnancy. Understanding what constitutes a high-risk pregnancy and how to manage it is crucial for ensuring the health and safety of both mother and baby.
Factors That Can Increase Pregnancy Risk
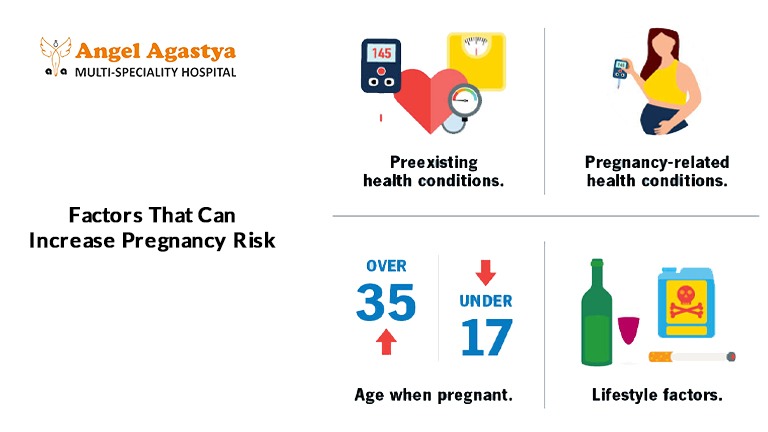
Several factors can increase the risk of pregnancy complications, making it essential for women to be aware of potential challenges and seek appropriate medical care. Some of these factors include:
1. Maternal Age
- Teenage Pregnancy: Teen pregnancies are considered high-risk pregnancies due to the physical and emotional immaturity of the mother. Teen mothers have a higher likelihood of developing complications such as preterm birth, low birth weight, and high blood pressure.
- Advanced Maternal Age: Pregnancies in women over 35 years of age are also considered high-risk pregnancies because of the increased likelihood of complications such as:
- Chromosomal Abnormalities: Conditions like Down syndrome occur more frequently in pregnancies of older mothers.
- Pregnancy Complications: Women over 35 are more susceptible to gestational diabetes, preeclampsia, and cesarean delivery due to increased pregnancy-related stress on the body.
2. Pre-existing Medical Conditions
Women with pre-existing medical conditions before pregnancy are at a higher risk of complications. Some of these conditions include:
- Chronic Diseases: Women with diabetes, hypertension, heart disease, kidney disease, autoimmune disorders (like lupus or rheumatoid arthritis), thyroid disorders, or certain blood disorders have a greater chance of developing pregnancy complications.
- Infections: Certain infections, such as HIV, hepatitis, and sexually transmitted infections (STIs), can significantly increase the risk of high-risk pregnancy complications for both the mother and the baby.
3. Pregnancy-Related Conditions
Even if a woman does not have pre-existing conditions, pregnancy itself can lead to health concerns that classify it as a high-risk pregnancy:
- Gestational Diabetes: This type of diabetes develops during pregnancy and can cause complications such as macrosomia (large babies), birth trauma, and future metabolic issues for the child.
- Preeclampsia: A serious condition characterized by high blood pressure and protein in the urine. Preeclampsia can lead to severe complications such as placental abruption, stroke, organ damage, and preterm delivery.
- Placental Abruption: This occurs when the placenta prematurely separates from the uterus, causing heavy bleeding and potential distress to the baby.
- Placenta Previa: A condition in which the placenta covers part or all of the cervix, leading to excessive bleeding and complications during labor.
- Multiple Pregnancies: Carrying twins, triplets, or more increases the risk of preterm labor, low birth weight, and gestational hypertension.
4. Obstetrical History
A history of previous pregnancy complications can increase the likelihood of a high-risk pregnancy in subsequent pregnancies. These complications may include:
- Preterm Birth
- Miscarriage
- Preeclampsia
- Cesarean Section (C-Section)
- Stillbirth
5. Lifestyle Factors
Certain lifestyle choices can contribute to a high-risk pregnancy:
- Smoking: Can increase the risk of low birth weight, preterm labor, and respiratory issues in newborns.
- Alcohol Consumption: Excessive alcohol intake can cause fetal alcohol spectrum disorders (FASDs), leading to developmental delays and birth defects.
- Drug Use: The use of illicit drugs can lead to congenital disabilities, premature birth, and withdrawal symptoms in newborns.
- Obesity: Obesity during pregnancy is linked to gestational diabetes, hypertension, and an increased risk of C-sections.
6. Environmental Factors
Exposure to environmental hazards such as toxic chemicals, radiation, or pollutants can negatively impact fetal development and contribute to a high-risk pregnancy.
Managing High-Risk Pregnancies

Women with high-risk pregnancies require close medical supervision and specialized care to minimize risks and ensure a successful pregnancy outcome.
1. Frequent Prenatal Checkups
Regular prenatal checkups, including ultrasounds, blood tests, and fetal monitoring, are crucial for tracking the health of both mother and fetus. These appointments help detect potential complications early, allowing for timely intervention.
2. Specialized Care
For severe high-risk pregnancies, a perinatologist (a doctor specializing in high-risk pregnancies) may be required. This specialist will closely monitor the pregnancy and develop a personalized management plan.
3. Lifestyle Modifications
Making lifestyle changes can significantly improve pregnancy outcomes:
- Eating a nutritious diet rich in fruits, vegetables, whole grains, and lean proteins
- Engaging in safe physical activities as recommended by a doctor
- Avoiding smoking, alcohol, and illicit drugs
- Maintaining a healthy weight
4. Medication and Treatment
Certain medications may be necessary to manage high-risk pregnancy complications:
- Blood Pressure Medications: For women with hypertension
- Insulin or Oral Medications: For women with gestational diabetes
- Blood Thinners: For women with a history of blood clots
5. Close Monitoring of Fetal Well-being
Regular fetal monitoring techniques include:
- Non-Stress Tests (NST): To track the baby’s heart rate.
- Biophysical Profiles (BPP): To assess fetal movements, amniotic fluid levels, and breathing patterns.
- Doppler Ultrasound: To check blood flow to the fetus.
Delivery Considerations in High-Risk Pregnancies

For some women with high-risk pregnancies, early delivery or a C-section may be necessary. Doctors may recommend early labor induction if they detect severe complications such as:
- Uncontrolled gestational diabetes
- Severe preeclampsia
- Fetal distress
NICU Support
In cases of preterm birth or other complications, babies may require neonatal intensive care unit (NICU) support after delivery to ensure their well-being.
Conclusion
A high-risk pregnancy requires specialized medical care, close monitoring, and proactive management to ensure the best outcomes for both mother and baby. By working closely with healthcare providers and adopting a healthy lifestyle, women with high-risk pregnancies can navigate the challenges successfully and give birth to healthy babies. If you are experiencing a high-risk pregnancy, it is essential to follow your doctor’s guidance and attend all scheduled checkups to minimize risks and ensure a safe delivery.
FAQs
1. What is a High-Risk Pregnancy?
A High-Risk Pregnancy is a pregnancy that poses increased health risks to the mother, the baby, or both. Various factors, such as maternal age, pre-existing health conditions, lifestyle choices, and pregnancy-related complications, can contribute to a High-Risk Pregnancy. Women experiencing a High-Risk Pregnancy require specialized medical care and close monitoring to ensure a safe delivery.
2. What are the common causes of High-Risk Pregnancy?
Several factors can lead to a High-Risk Pregnancy, including advanced maternal age (over 35), teenage pregnancy, pre-existing medical conditions like diabetes or hypertension, multiple pregnancies (twins or more), obesity, and pregnancy-related complications such as gestational diabetes and preeclampsia. Lifestyle factors like smoking, drug use, and excessive alcohol consumption can also contribute to a High-Risk Pregnancy.
3. How can I know if I have a High-Risk Pregnancy?
Your doctor will assess your health history, lifestyle, and any existing medical conditions to determine if you have a High-Risk Pregnancy. Regular prenatal checkups, ultrasound scans, blood tests, and fetal monitoring can help detect potential risks early. If you have a history of complications in previous pregnancies, your doctor may classify your current pregnancy as a High-Risk Pregnancy.
4. What complications are associated with a High-Risk Pregnancy?
A High-Risk Pregnancy can lead to complications such as preterm labor, low birth weight, gestational diabetes, preeclampsia, placental abruption, and fetal distress. In severe cases, a High-Risk Pregnancy may increase the likelihood of a cesarean section (C-section) or require immediate medical intervention to protect the health of both the mother and baby.
5. Can a High-Risk Pregnancy be prevented?
While not all cases of High-Risk Pregnancy can be prevented, adopting a healthy lifestyle, managing pre-existing health conditions, attending regular prenatal checkups, and avoiding harmful substances like tobacco and alcohol can significantly lower the risks. Proper prenatal care and early detection of potential complications can help manage a High-Risk Pregnancy effectively.
6. How is a High-Risk Pregnancy managed?
Managing a High-Risk Pregnancy involves frequent prenatal checkups, specialized care from high-risk pregnancy experts (perinatologists), lifestyle modifications, and medication when necessary. Doctors may recommend close fetal monitoring, dietary adjustments, stress management, and bed rest in some cases to ensure a safe pregnancy.
7. Do all High-Risk Pregnancies require a cesarean section?
Not all High-Risk Pregnancies require a cesarean section. Many women with a High-Risk Pregnancy can have a normal vaginal delivery if their condition is well-managed. However, in cases where complications arise, such as fetal distress, placenta previa, or severe preeclampsia, a C-section may be the safest option for both mother and baby.
8. What lifestyle changes can help during a High-Risk Pregnancy?
Women experiencing a High-Risk Pregnancy should maintain a nutritious diet, engage in doctor-approved physical activity, stay hydrated, manage stress levels, and avoid smoking, alcohol, and drugs. Proper sleep, prenatal vitamins, and regular medical checkups play a crucial role in ensuring a healthy outcome in a High-Risk Pregnancy.
9. Can I have a healthy baby with a High-Risk Pregnancy?
Yes, many women with a High-Risk Pregnancy go on to have healthy babies. With proper medical care, lifestyle adjustments, and regular monitoring, most complications can be managed effectively. Open communication with healthcare providers and following their recommendations will increase the chances of a successful pregnancy outcome.
10. When should I see a specialist for a High-Risk Pregnancy?
If you have a pre-existing medical condition, are over 35, have had complications in previous pregnancies, or experience symptoms like severe swelling, high blood pressure, or unusual pain, you should consult a high-risk pregnancy specialist (maternal-fetal medicine specialist). Early intervention and expert guidance can help ensure the best possible outcome for a High-Risk Pregnancy.

