Exploring the Endometriosis-Autoimmune Link: What Science Reveals
Are you dealing with unexplained pain, fatigue, or digestive issues? Recent studies reveal an intriguing connection between endometriosis and autoimmune disorders, shedding light on shared symptoms, underlying mechanisms, and potential therapies. This emerging understanding of the endometriosis-autoimmune link offers hope for millions affected by these chronic conditions.
Introduction

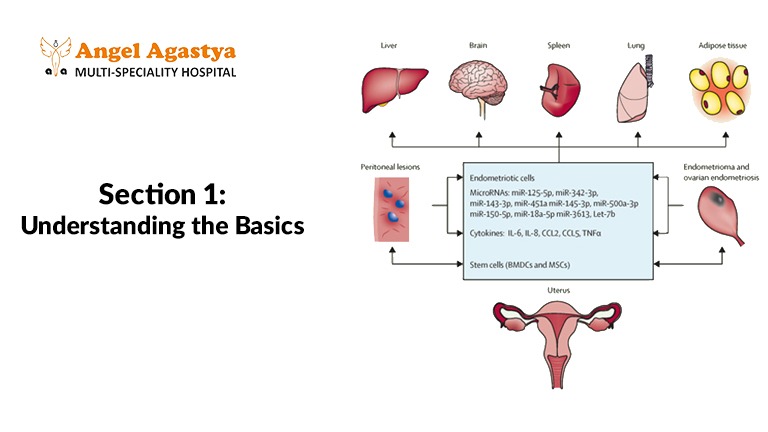
The endometriosis-autoimmune link has become a critical focus of research in recent years. Endometriosis, a chronic inflammatory condition, involves the growth of tissue similar to the uterine lining (endometrium) outside the uterus. This misplaced tissue causes a cascade of problems, including severe pain, infertility, and systemic inflammation.
Similarly, autoimmune disorders occur when the immune system mistakenly attacks the body’s healthy tissues, leading to widespread inflammation and damage. Conditions like lupus, rheumatoid arthritis, and Hashimoto’s thyroiditis are some examples of autoimmune diseases.
Although the exact causes of endometriosis and autoimmune disorders remain unclear, significant overlaps in symptoms, immune dysfunction, and inflammation have led researchers to investigate the endometriosis-autoimmune link further. Understanding this connection could transform diagnostic approaches, treatments, and ultimately the quality of life for those affected.
Endometriosis: A Closer Look
To understand the endometriosis-autoimmune link, we must first grasp what endometriosis entails.
Endometriosis occurs when tissue resembling the uterine lining grows outside the uterus, typically attaching to organs like the ovaries, fallopian tubes, and pelvic lining. In rare cases, it may spread to distant organs, such as the lungs. This tissue responds to hormonal changes during menstruation but has no way to leave the body. The result is:
- Chronic inflammation
- Formation of scar tissue (adhesions)
- Severe pain and complications
Symptoms of Endometriosis

Endometriosis symptoms can vary greatly from person to person, but some of the most common include:
- Intense pelvic pain, especially during menstruation, often described as sharp or cramp-like.
- Heavy periods (menorrhagia), where bleeding is unusually heavy and prolonged.
- Painful intercourse (dyspareunia), which can lead to discomfort or pain during or after sex.
- Fatigue, often severe, affecting daily activities and energy levels.
- Infertility, which is a common concern for those diagnosed with endometriosis.
- Digestive issues, such as bloating, constipation, and diarrhea, which are often mistaken for conditions like irritable bowel syndrome (IBS).
The interplay between immune dysfunction and chronic inflammation has made the endometriosis-autoimmune link a subject of great interest in the medical community.
Autoimmune Disorders: A Snapshot
Autoimmune disorders occur when the immune system mistakenly identifies healthy tissues as threats. This misfire triggers a series of immune responses that cause chronic inflammation and tissue damage.
Common Autoimmune Disorders
- Lupus: A systemic autoimmune disease affecting the skin, joints, and organs.
- Rheumatoid Arthritis: Inflammation primarily targeting the joints.
- Celiac Disease: An immune response to gluten that damages the small intestine.
- Hashimoto’s Thyroiditis: An autoimmune condition targeting the thyroid gland.
The immune system’s behavior in autoimmune disorders mirrors the irregularities observed in endometriosis. This overlap strengthens the case for an endometriosis-autoimmune link.
The Overlapping Symptoms
The endometriosis-autoimmune link is evident in the way these conditions share numerous symptoms, which can lead to delays or errors in diagnosis.
Chronic Pain
- Endometriosis: Often presents with debilitating pelvic pain during menstruation, as well as pain in the back, bladder, and legs.
- Autoimmune Disorders: Conditions like lupus and rheumatoid arthritis cause joint pain, muscle aches, and widespread pain.
Fatigue
Fatigue is a hallmark of both endometriosis and autoimmune disorders. Chronic inflammation, disrupted sleep patterns due to pain, and immune system dysfunction contribute to persistent exhaustion.
Digestive Problems
The endometriosis-autoimmune link extends to gastrointestinal symptoms. Digestive issues like bloating, diarrhea, constipation, and nausea are:
- Endometriosis: Commonly mistaken for IBS.
- Autoimmune Disorders: Frequently seen in conditions like celiac disease and Crohn’s disease.
Skin Manifestations
- Autoimmune Disorders: Skin rashes, photosensitivity, or lesions are common in lupus and other autoimmune diseases.
- Endometriosis: Although less common, some women with endometriosis report skin conditions like eczema or acne, suggesting a possible immune link.
The Immune System Connection

The immune system plays a central role in the endometriosis-autoimmune link. Let’s examine how.
Immune Dysfunction in Endometriosis
In a healthy body, the immune system functions by identifying and eliminating abnormal cells or tissue that could cause harm. However, in endometriosis, this process is disrupted.
The immune system fails to recognize and properly remove the endometrial-like tissue that grows outside the uterus.
This dysfunction leads to chronic inflammation, which creates an environment where lesions can thrive and cause further damage. This immune failure contributes to the persistent pain and complications experienced by individuals with endometriosis.
Autoimmune Mechanisms at Play
In autoimmune disorders, the immune system mistakenly attacks the body’s healthy tissues. Researchers believe the endometriosis-autoimmune link reflects similar immune dysfunction, which may worsen symptoms or increase the risk of developing both conditions.
Chronic Inflammation: The Common Thread
Chronic inflammation is a central factor in both endometriosis and autoimmune disorders. In these conditions, the immune system becomes overactive, leading to prolonged inflammation that negatively impacts the body. This ongoing inflammation perpetuates a range of symptoms, including
Pain:often severe and persistent.
It also contributes to tissue damage, as the immune system mistakenly attacks healthy tissues. Additionally, chronic inflammation accelerates disease progression, making the conditions harder to manage over time. Effective management of inflammation is crucial for controlling symptoms and preventing further harm in individuals suffering from endometriosis and autoimmune diseases.
- Pain:Often severe and persistent
- Tissue damage:It also contributes to tissue damage,as the immune system mistakenly attacks healthy tissues.
- Disease progression:chronic inflammation accelerates disease progression, making the conditions harder to manage over time.
Effective management of inflammation is crucial for controlling symptoms and preventing further harm in individuals suffering from endometriosis and autoimmune diseases.The endometriosis-autoimmune link highlights how unchecked inflammation in these conditions can lead to systemic effects, making treatment more challenging.
Diagnostic Challenges

The overlapping symptoms complicate the diagnosis of endometriosis and autoimmune disorders, often leading to years of misdiagnoses.
Diagnosing Endometriosis
- Pelvic Exams: Can reveal abnormalities but are often inconclusive.
- Imaging Tests: Ultrasounds and MRIs detect large cysts but frequently miss smaller lesions.
- Laparoscopy: The gold standard, allowing direct visualization and biopsy of lesions.
Diagnosing Autoimmune Disorders
- Blood Tests: Inflammation markers like CRP (C-reactive protein) and ANA (antinuclear antibodies) are common diagnostic tools.
- Specialized Tests: Include rheumatoid factor for arthritis and tTG antibodies for celiac disease.
The endometriosis-autoimmune link underscores the importance of comprehensive diagnostic approaches.
Treatment Strategies
While no cure exists for either condition, understanding the endometriosis-autoimmune link has informed strategies for managing symptoms and improving quality of life.
Medical Treatments
- Pain Management: NSAIDs and prescription pain relievers.
- Hormonal Therapy:
- Birth control pills or IUDs for endometriosis to suppress tissue growth.
- Immunosuppressants:
- Common in autoimmune disorders to reduce immune system overactivity.
Surgical Options
For severe endometriosis, laparoscopy or excision surgery can remove lesions, alleviate pain, and improve fertility outcomes.
Lifestyle and Holistic Approaches
Lifestyle interventions play a vital role in managing the endometriosis-autoimmune link.
Anti-Inflammatory Diet
- Focus on whole foods: fruits, vegetables, lean proteins, and omega-3 fatty acids.
- Avoid processed foods, sugars, and potential triggers like gluten.
Stress Management
Chronic stress exacerbates inflammation. Techniques such as:
- Yoga
- Meditation
- Deep breathing exercises
can significantly reduce stress and support healing.
Regular Physical Activity
Low-impact activities like walking, swimming, or Pilates can help manage stiffness, pain, and fatigue.
The Future of Research

As scientists delve deeper into the endometriosis-autoimmune link, exciting possibilities for targeted treatments and personalized care are emerging.
Genetic and Immune Pathways
Research aims to uncover:
- Shared genetic predispositions.
- Common immune pathways driving both conditions.
Innovative Therapies
Emerging treatments include:
- Biologics targeting specific immune pathways.
- Personalized medicine based on individual genetic and immune profiles.
Conclusion
The endometriosis-autoimmune link highlights a critical intersection of two complex conditions. By understanding shared symptoms, immune dysfunction, and the role of chronic inflammation, researchers and healthcare providers can work towards more effective, personalized treatments.
For individuals navigating these challenges, raising awareness and embracing a holistic approach that combines medical care, lifestyle changes, and emerging therapies can improve outcomes and quality of life.
FAQs About the Endometriosis-Autoimmune Link
What symptoms indicate the endometriosis-autoimmune link?
Shared symptoms include chronic pain, fatigue, digestive issues, and skin conditions.
2.How is the link between these conditions diagnosed?
Endometriosis often requires laparoscopy, while autoimmune disorders rely on blood tests and clinical evaluation.
3.Can lifestyle changes improve symptoms?
Yes, an anti-inflammatory diet, stress management, and regular exercise can significantly reduce symptoms.
4.What is the role of inflammation in these conditions?
Chronic inflammation drives pain, tissue damage, and disease progression in both endometriosis and autoimmune disorders.
5.What are the future prospects for treatment?
Targeted therapies and personalized medicine are promising areas of ongoing research.
6.What are some common autoimmune diseases that may be linked to endometriosis
Lupus, rheumatoid arthritis, celiac disease, and Hashimoto’s thyroiditis.
7.How is endometriosis diagnosed?
Diagnosis often involves pelvic exams, imaging tests like ultrasounds and MRIs, and laparoscopy for definitive diagnosis.
8.How are autoimmune diseases diagnosed?
Diagnosis typically involves blood tests, physical examinations, and sometimes specialized tests.
9.Is there a genetic link between endometriosis and autoimmune diseases?
Research suggests a possible genetic predisposition to both conditions.
10.How can I improve my quality of life if I have endometriosis or an autoimmune disease?
By working closely with your healthcare provider, managing stress, adopting a healthy lifestyle, and exploring complementary therapies.

