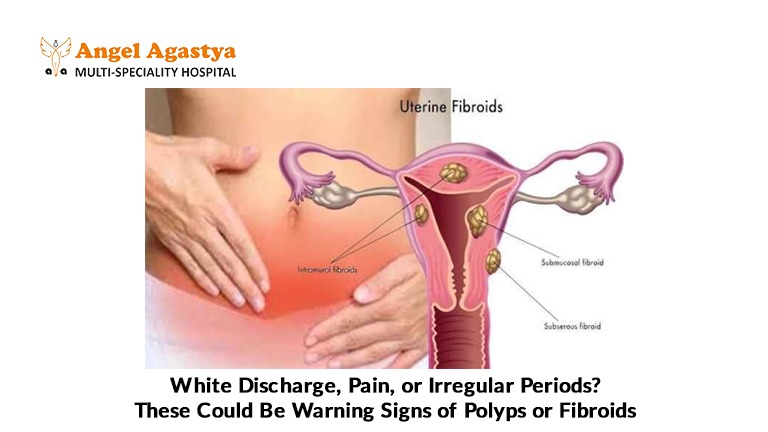
White Discharge, Pain or Irregular Periods? These Could Be Warning Signs of Polyps or Fibroids
Noticing irregular periods, unusual white discharge, or pelvic pain? These symptoms may be more than just hormonal shifts. They could point to uterine polyps or fibroids common yet often overlooked. Let’s uncover what your body might be trying to tell you.
Are you navigating the complexities of your menstrual cycle, only to be met with unsettling changes? Perhaps you’ve noticed an unusual white discharge, a persistent ache in your pelvis, or the frustrating inconsistency of irregular periods. While the female body experiences a range of fluctuations, the simultaneous occurrence of these symptoms, particularly when your periods become unpredictable, could be your body’s subtle yet significant way of raising a red flag. It’s easy to dismiss these changes as minor inconveniences, but understanding their potential connection to conditions like uterine polyps or fibroids is crucial for your well-being.
Let’s embark on a journey to unravel the potential links between irregular periods, that persistent white discharge, nagging pelvic pain, and the possibility of these often benign, yet sometimes troublesome, uterine growths. Are these symptoms causing a ripple of concern in your mind? If so, continue reading. This exploration will shed light on these conditions and guide you on when seeking professional medical advice becomes an essential step towards safeguarding your health.
Decoding the Rhythm: Understanding Irregular Periods
To truly understand when your menstrual cycle might be signaling an underlying issue, it’s important to first establish a baseline of what constitutes a “normal” rhythm. Typically, a menstrual cycle spans approximately 21 to 35 days, counted from the first day of one period to the first day of the next. The flow itself usually lasts between 2 to 7 days and occurs with a predictable regularity each month.

Irregular periods, on the other hand, deviate from this predictable pattern. This can manifest in various ways: your cycle length might fluctuate significantly from month to month, you might experience skipped periods altogether, or you might notice an unusual heaviness or lightness in your menstrual flow. Spotting between periods, bleeding after intercourse, or periods that last for an abnormally long time also fall under the umbrella of menstrual irregularities.
It’s worth noting that occasional irregularities can be attributed to a myriad of factors. Stress, significant weight changes, intense exercise, hormonal fluctuations during puberty or perimenopause, and even certain medications can temporarily disrupt your cycle. However, when these irregularities become a consistent pattern, especially when accompanied by other concerning symptoms, it’s time to pay closer attention.
When the Unpredictable Becomes a Cause for Concern: The Symptom Cluster
While an isolated instance of a late period might not be alarming, the confluence of irregular periods with other symptoms like unusual white discharge and pelvic pain warrants a more thorough investigation. This is where the possibility of uterine polyps or fibroids comes into play.
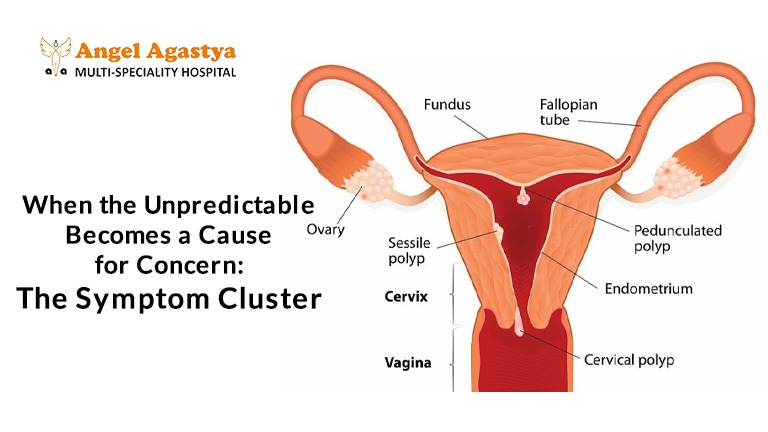
Uterine Polyps: Small Growths, Notable Impact
Uterine polyps are small, finger-like growths that develop in the lining of the uterus (endometrium). These benign growths can vary in size, from a few millimeters to several centimeters. While many polyps remain asymptomatic, they can often disrupt the normal shedding of the uterine lining, leading to irregular bleeding patterns.
One of the hallmark symptoms of uterine polyps is irregular bleeding, which can present as spotting between your regular periods, heavier than usual menstrual flow, prolonged periods, or even bleeding after menopause. Additionally, polyps can sometimes cause an increase in vaginal discharge, which might appear white or clear. While pain is less commonly associated with polyps, larger polyps or those located near the cervix can occasionally cause discomfort or cramping. The exact causes of uterine polyps aren’t fully understood, but hormonal factors, particularly high levels of estrogen, are believed to play a role. Risk factors include being perimenopausal or postmenopausal, having high blood pressure, or being obese.
Uterine Fibroids: Size Matters in Their Influence
Uterine fibroids, also known as leiomyomas, are non-cancerous tumors that grow within the muscle tissue of the uterus. These are incredibly common, affecting a significant percentage of women by the time they reach menopause. Fibroids can vary dramatically in size, ranging from tiny, undetectable nodules to large masses that can distort the shape of the uterus.
The impact of fibroids on your menstrual cycle and overall well-being largely depends on their size, number, and location within the uterus. They can significantly disrupt the uterine lining and blood supply, often leading to irregular and heavy menstrual bleeding, sometimes accompanied by the passage of clots. The increased bleeding can, in some cases, contribute to an increase in vaginal discharge. Furthermore, larger fibroids can exert pressure on surrounding organs, causing pelvic pain, a feeling of fullness or heaviness in the lower abdomen, backache, and even frequent urination or constipation. While the exact cause of fibroids is unknown, hormonal influences, particularly estrogen and progesterone, and genetic factors are thought to be involved. Risk factors include age (being in your 30s and 40s), being of African descent, a family history of fibroids, obesity, and early onset of menstruation.
White Discharge and Pelvic Pain: Signals That Amplify Concern
While normal vaginal discharge is typically clear or whitish, odorless, and varies throughout your menstrual cycle, changes in its characteristics can be indicative of an underlying issue. An increase in white discharge, particularly if it’s accompanied by a foul odor, itching, or irritation, could signal an infection. However, in the context of irregular periods and pelvic pain, it can also be associated with hormonal imbalances or the presence of polyps or fibroids.
Pelvic pain associated with polyps might be mild or intermittent, often described as cramping. In contrast, fibroid-related pain can range from a dull, persistent ache or pressure in the pelvic region to sharp, intense pain during menstruation, especially with larger fibroids. The location and type of pain can offer clues about the potential underlying cause.
It’s crucial to remember that white discharge and pelvic pain can have numerous other causes, including infections, endometriosis, or other gynecological conditions. However, their co-occurrence with irregular periods significantly elevates the need for a thorough medical evaluation to rule out conditions like polyps and fibroids.
The Importance of Timely Diagnosis: Paving the Way for Effective Management
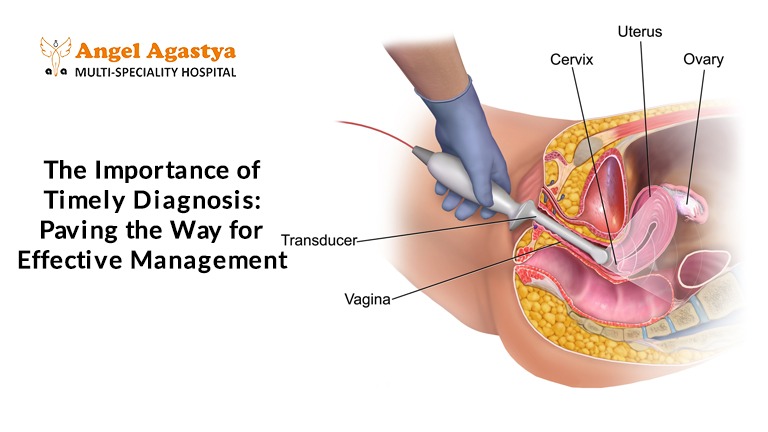
Ignoring persistent or concerning symptoms can delay diagnosis and potentially lead to complications. Seeking timely medical attention is paramount when you experience a combination of irregular periods, unusual white discharge, and pelvic pain. A gynecological examination, which may include a pelvic exam, ultrasound (to visualize the uterus and ovaries), and potentially a hysteroscopy (a procedure where a thin, lighted tube is inserted into the uterus to examine its lining), are crucial diagnostic tools. Early diagnosis allows for the prompt initiation of appropriate management strategies, preventing potential complications such as anemia due to heavy bleeding or, in rare cases, the overlooking of more serious conditions.
Navigating Treatment Options: Tailored to Your Needs
The approach to managing uterine polyps and fibroids varies depending on factors such as the size, number, and location of the growths, the severity of your symptoms, your age, and your future reproductive plans. Treatment options can range from watchful waiting (if symptoms are mild) to medical therapies aimed at shrinking fibroids or managing symptoms, and surgical interventions such as polypectomy (removal of polyps) or myomectomy (removal of fibroids) or, in some cases, hysterectomy (removal of the uterus). Your healthcare provider will discuss the most suitable options based on your individual circumstances.
When to Seek Expert Care: Listen to Your Body’s Signals
It’s essential to be proactive about your gynecological health. Don’t hesitate to seek medical attention if you experience any of the following:
- Sudden and significant changes in your menstrual flow.
- Unusually heavy bleeding that requires frequent changes of pads or tampons.
- Bleeding between your regular periods or after menopause.
- Persistent pelvic pain that interferes with your daily activities.
- Unusual or foul-smelling vaginal discharge.
Consulting a gynecologist will provide you with an accurate diagnosis and a personalized care plan tailored to your specific needs.
Experience World-Class Care at Angel Agastya Hospital: Your Partner in Women’s Health
At Angel Agastya Hospital, we understand the unique healthcare needs of women. We are committed to providing world-class care at Angel Agastya, where advanced treatments, compassionate staff, and a healing environment come together to support your journey to better health.

Our dedicated team of experienced gynecologists offers comprehensive and personalized care for a wide range of conditions, including menstrual irregularities, uterine polyps, and fibroids. From normal deliveries to high-risk pregnancies, we offer personalized care. We utilize advanced gynecology, including state-of-the-art diagnostic tools and minimally invasive surgical techniques, to ensure accurate diagnosis and effective treatment. Our commitment extends to infertility treatments, endoscopy, and safe surgeries, ensuring your health and comfort every step of the way.
If you are experiencing irregular periods, white discharge, pelvic pain, or have any gynecological concerns, we encourage you to seek expert consultation at Angel Agastya Hospital. Our compassionate and skilled team is here to provide you with comprehensive care and support, guiding you towards optimal health and well-being.
Empowering Your Health Journey: Knowledge is Key
Understanding the potential significance of symptoms like irregular periods, unusual white discharge, and pelvic pain is the first step towards proactive health management. By being aware of your body’s signals and seeking timely medical advice when needed, you empower yourself to take control of your well-being. Remember, you don’t have to navigate these concerns alone. Reach out to healthcare professionals who can provide the guidance and care you deserve.
Frequently Asked Questions (FAQ)
1. What are uterine polyps and fibroids?
Uterine polyps are small, non-cancerous growths in the uterine lining, while fibroids are benign tumors in the muscle layer of the uterus. Both can affect your periods and cause discomfort.
2. How can I tell if my periods are irregular?
If your cycle length keeps changing, you skip periods, or experience unusually heavy or light flow, your periods may be irregular.
3. Is white discharge always a cause for concern?
Not always. Normal discharge is usually clear or white and odorless. But if it’s excessive, has a foul smell, or comes with pain or itching, it may signal a problem.
4. What are the warning signs of polyps or fibroids?
Look out for irregular periods, heavy bleeding, white discharge, pelvic pain, or bleeding between periods.
5. Can polyps or fibroids affect fertility?
Yes. In some cases, they can interfere with conception or pregnancy, depending on their size and location.
6. What causes these growths to develop?
Hormonal imbalances, especially high estrogen, as well as age, genetics, obesity, and early menstruation can increase the risk.
7. When should I see a gynecologist?
If you have ongoing irregular periods, unusual discharge, persistent pelvic pain, or bleeding between periods, it’s time to consult a doctor.
8. What tests help diagnose polyps or fibroids?
Doctors may use ultrasounds, pelvic exams, or hysteroscopy to get a clear diagnosis.
9. Are treatments for fibroids and polyps always surgical?
Not always. Depending on symptoms, you may need only monitoring, medications, or minor procedures. Surgery is an option if the growths are large or causing major issues.
10. Can lifestyle changes help manage symptoms?
Yes. Maintaining a healthy weight, managing stress, and tracking your cycle can support your overall reproductive health.

