“Endometriosis After Menopause: Unveiling Risks and Powerful Relief Options”
“Think menopause means the end of endometriosis? Think again. Learn how to manage symptoms and reclaim control over your health.”
Introduction
Endometriosis after Menopause is often an overlooked topic, as most associate this condition with reproductive years. However, endometriosis after menopause is not only possible but can also affect overall health significantly. While menopause usually signifies a drop in estrogen levels, some women still experience the condition due to various factors, such as hormone replacement therapy (HRT). This guide delves into the persistence of endometriosis after menopause, its symptoms, risks, and available treatments.
This blog explores how endometriosis manifests beyond menopause, the associated risks, and the treatment options available. By shedding light on this often-overlooked phase, we aim to provide valuable insights for women navigating this condition in their later years.
Understanding Endometriosis
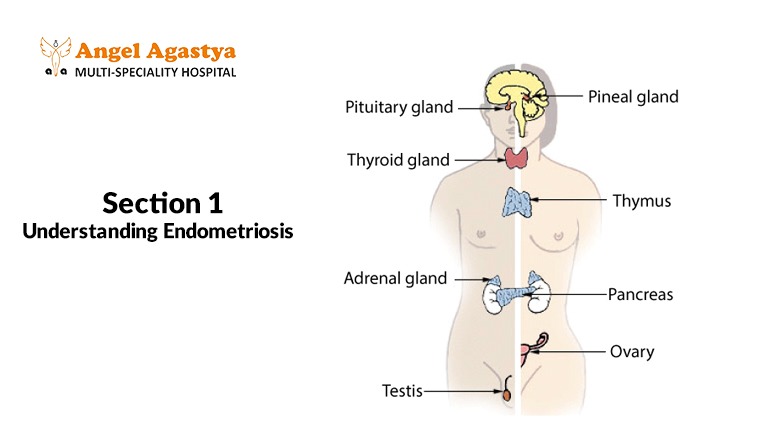
What is Endometriosis?
In essence, endometriosis refers to the persistence of tissue resembling the uterine lining, growing in areas outside the uterus. This can lead to chronic pain and complications even after estrogen levels decrease.
The Role of Hormones
Hormones, especially estrogen, fuel the growth of endometrial tissue. For women dealing with endometriosis treatments like HRT can reintroduce estrogen into the body, potentially triggering or worsening symptoms.
Endometriosis After Menopause
Persistence of Endometriosis
For many women, endometriosis doesn’t mean relief. Residual endometrial implants may remain active, causing pain and inflammation.While menopause brings hormonal changes that often alleviate endometriosis symptoms, it doesn’t guarantee their complete disappearance. Some women with severe or widespread disease may continue to experience pain and other related symptoms due to residual endometrial implants.
Development of Endometriosis Post-Menopause
Though rare, some women may develop endometriosis for the first time. This phenomenon is usually associated with the use of HRT, which reintroduces estrogen into the body. Estrogen can stimulate dormant endometrial cells, causing them to become active and symptomatic again.
Symptoms of Endometriosis After Menopause
Women experiencing endometriosis after menopause report various symptoms, such as:
- Chronic Pelvic Pain
Persistent pain in the lower abdomen or Chronic pelvic pain is a hallmark of endometriosis, often stemming from residual inflammation or scar tissue. - Painful Intercourse
For some, this leads to discomfort during or after sexual intercourse due to adhesions in the pelvic area. - Digestive Issues
Symptoms like bloating and constipation are not uncommon in women with endometriosis exacerbated by hormonal or dietary factors.Endometriosis can also affect the digestive system, leading to bloating, diarrhea, or constipation. For postmenopausal women, these issues might be exacerbated by coexisting conditions or treatments like HRT
Health Risks Associated with Endometriosis After Menopause
Increased Risk of Cancer
Studies have shown that women with a history of endometriosis after menopause may face a higher risk of developing certain cancers, particularly ovarian and endometrial cancers. Though the overall risk remains low, postmenopausal women should discuss regular screenings and monitoring with their healthcare providers.
Chronic Pain
Untreated or poorly managed endometriosis after menopause can lead to persistent pain ,affecting mental health and daily life . This pain might contribute to sleep disturbances, mental health issues like anxiety or depression, and reduced daily functioning.
Impact on Fertility
For postmenopausal women considering assisted reproductive techniques like egg donation, endometriosis after menopause can pose challenges. Severe cases involving scarring or adhesions may impact the success rates of such procedures.
Diagnosing Endometriosis Post-Menopause
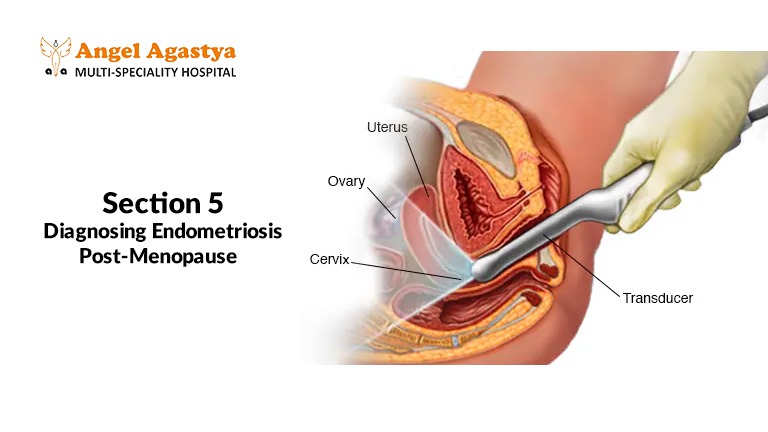
Diagnosing endometriosis after menopause can be challenging. Symptoms often overlap with other conditions common in older women, such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID). Diagnostic methods include:
- Imaging Tests: Ultrasound or MRI scans may detect endometrial implants or ovarian cysts.
- Laparoscopy: A minimally invasive surgical procedure that allows direct visualization and potential biopsy of endometrial tissue.
- Blood Tests: While not definitive, certain markers like CA-125 may provide clues in advanced cases.
Treatment Options for Endometriosis After Menopause

1. Hormone Therapy
HRT, while effective in managing menopausal symptoms like hot flashes or bone density loss, can also exacerbate endometriosis after menopause if not monitored carefully . Healthcare providers must carefully balance the benefits and risks when prescribing HRT to women with a history of endometriosis.
2. Surgical Intervention
Surgery may be considered for women with severe symptoms or complications like bowel obstruction. Options include excision surgery to remove endometrial implants or, in extreme cases, a hysterectomy with removal of the ovaries.
3. Pain Management Chronic pain can be managed through:
- Over-the-counter analgesics like ibuprofen or acetaminophen.
- Prescription medications, including neuropathic pain relievers or hormonal treatments.
- Alternative therapies, such as acupuncture, physical therapy, or mindfulness techniques.
4. Lifestyle and Natural Remedies
- Dietary Changes: Anti-inflammatory diets rich in omega-3 fatty acids, fruits, and vegetables may alleviate symptoms of endometriosis after menopause.
- Regular Exercise: Activities like yoga or Pilates can improve flexibility, reduce stress, and manage pain.
- Stress Management: Meditation, counseling, or joining support groups can help cope with the emotional burden of chronic conditions.
Emotional and Psychological Impact

Endometriosis after menopause isn’t merely a physical condition—it can deeply impact mental health. Postmenopausal women dealing with persistent symptoms often feel isolated or misunderstood. Acknowledging this emotional toll is essential:
- Support Groups: Engaging with other women who have similar experiences can offer valuable support and coping strategies.
- Counseling Services: Professional therapy can help address anxiety, depression, or relationship strains arising from the condition.
Prevention and Proactive Measures
While it’s not always possible to prevent endometriosis after menopause , adopting a proactive approach can mitigate risks:
- Early Diagnosis: Recognizing symptoms early and seeking medical advice can prevent complications.
- Informed Choices about HRT: Discuss potential risks and benefits of hormone therapy with your doctor if you’re postmenopausal and have a history of endometriosis.
- Regular Checkups: Routine pelvic exams and screenings for gynecological health are vital, especially for women with a history of the condition.
Conclusion
Endometriosis after Menopause is a condition that requires attention and care. With proper diagnosis, treatment, and lifestyle changes, women can manage symptoms effectively. By raising awareness about endometriosis after menopause, we empower women to seek timely help and improve their quality of life.
It is a lesser-known yet significant aspect of this condition that deserves attention. Understanding its potential persistence, symptoms, and health risks empowers women to seek appropriate care. Through timely diagnosis, tailored treatment, and holistic management strategies, postmenopausal women can lead fulfilling lives despite the challenges posed by endometriosis after menopause . By raising awareness about endometriosis after menopause we empower women to seek timely help and improve their quality of life.
If you or someone you know is navigating endometriosis after menopause, remember that support and solutions are available. Collaborate with healthcare providers, explore treatment options, and prioritize your well-being to reclaim control over your health and happiness.
FAQs
1. Can endometriosis worsen later in life?
Yes, especially in cases linked to hormone replacement therapy (HRT).
2. What are the signs of endometriosis in postmenopausal women?
Common signs include persistent pelvic pain, painful intercourse, fatigue, and digestive discomfort.
3. Does this condition increase cancer risks?
There is a slight increase in the risk of ovarian and endometrial cancers among women with this condition.
4. What treatment options are available for this condition in later years?
Treatment may involve hormone therapy, surgery, pain management techniques, and lifestyle modifications.
5. Can stress and lifestyle choices impact symptoms?
Yes, stress and lifestyle factors can influence symptom severity. Stress management and anti-inflammatory diets can be beneficial.
6. Are there natural ways to ease the discomfort?
Yes, strategies like dietary adjustments, regular exercise, and therapies such as acupuncture may help alleviate symptoms.
7. How is this condition diagnosed in older women?
Diagnosis often involves imaging studies, laparoscopy, and specific blood tests.
8. Can hormone therapy influence this condition?
Hormone replacement therapy can sometimes trigger or worsen symptoms in postmenopausal women.
9 .What is the long-term prognosis for women managing this condition post-menopause?
With effective treatment, most women can enjoy a pain-free and healthy lifestyle.
10. Where can one find support for this condition?
Support groups are available through online forums, local healthcare organizations, and specialized clinics.

